
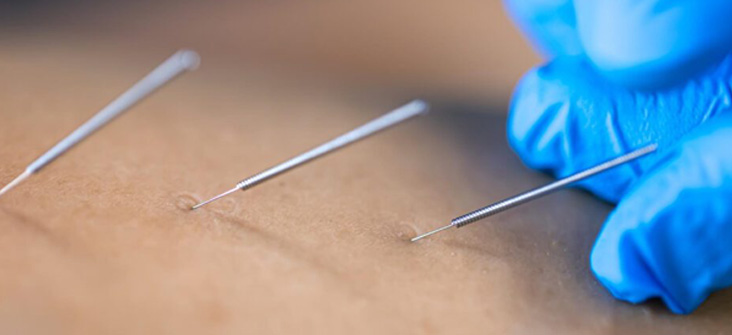
Dry needling is when a thin needle is strategically inserted into or near trigger points, prompting muscle contractions and twitches, ultimately leading to pain relief and improved range of motion. This therapeutic approach aims to alleviate pain and address movement issues associated with myofascial trigger points, but it is not without its risks. Healthcare providers considering this treatment must be acutely aware of the potential complications for their patients.
An insured noted a dry needling accident which occurred at her practice on 6 February 2020, resulting in Plaintiff suffering a pneumothorax. Before the treatment, informed consent was brought to the Plaintiff’s attention.
Whilst there is possible merit in respect of the negligence which caused the pneumothorax, the amount claimed is debatable, particularly that “the plaintiff will experience mental anguish requiring the plaintiff to undergo psychotherapy”. Medical substantiation is needed.
An insured treated a patient with dry needling for neck pain. A couple of days after treatment, the patient started to feel faint and felt like her legs were giving in. She subsequently went to the emergency room. The attending doctor ordered an MRI which allegedly showed severe damage to the nerve, and which they have attributed to the dry needling performed by the Insured.
Given the invasive nature of dry needling, obtaining informed consent from patients is required.


